Designing Trust into Telemedicine
How UX Research drove a 70% rise in video consultations
Role
UX Research Lead
Goal
Understand barriers to teleconsultation and increase user adoption
Method
• 24 in-depth interviews
• 3 user archetypes
• 1 feature roadmap
Outcome
70% increase in teleconsultation use
over 3 years
Turning User Hesitation into Product Growth
When users skipped the “Consult a Doctor” option, the client assumed it was a marketing issue. But my
UX research revealed a deeper story: the lack of emotional trust in remote care. I led research to uncover users' mental models, design confidence-building touchpoints, and help reshape product strategy, contributing to a 70% increase in adoption of video consultations over 3 years.
01. The Challenge
Business Challenge
The organization wanted to increase adoption of its video consultation feature, a core offering intended to make healthcare more accessible and scalable. Although the feature had been live for over a year, uptake remained significantly lower than expected. The business saw this as a missed opportunity for growth and wanted to understand what was holding users back, so future investments in the platform could better align with user needs.
User Experience Challenge
While the feature was technically functional and easy to locate within the app, adoption lagged. What wasn’t clear was why users weren’t choosing it. There were no obvious usability bugs, but something was preventing users from moving forward.

As the UX researcher, I was brought in to explore this gap specifically:

What were the perceived risks or doubts around
video consultations?

How did users make healthcare decisions in this digital context?

What were the expectations users had from remote care?

And what design levers could reduce hesitation and build confidence?
The goal was not just to identify barriers, but to uncover the emotional and cognitive factors shaping behavior and translate those insights into actionable design and communication strategies.
02. Research Strategy
To uncover what drives trust in telemedicine and how to design for user confidence, I structured the study into two phases. This ensured we moved from understanding user attitudes to co-creating design solutions grounded in real user needs.
Phase 1
Phase 2
Goal: What users expect from remote care
Methods: Co-creation and Validation
Goal: What drives trust?
Methods: Contextual Inquiry, Interviews
Output: Mental Models, Personas
Output: Design Levers, Feature Mapping
Digging deeper into Phase 1
Understanding What Builds Trust
Why this phase
Before designing solutions, it was essential to understand what makes users trust a doctor - both offline and online. If we could identify the signals that build confidence in physical consultations, we could replicate or adapt them for a digital experience.
Interview Focus Areas - Semi-Structured, Exploratory




Healthcare Decision Triggers
How do users select a doctor offline?
What cues signal credibility?
(e.g., referrals
clinic reputation)
Trust
Drivers
What reassures them about diagnosis accuracy during in-person visits?
Trust Cues in Digital Context
What would help them feel the same level of trust online?
Adoption
Barriers
What concerns or doubts stop them from trying telemedicine?
What This Phase Delivered
-
Mental models of trust-building, comparing offline and online care
-
3 Personas, each representing distinct attitudes, trust thresholds, and comfort levels—forming the foundation for Phase 2
Digging deeper into Phase 2
Designing for User Expectations
Why this phase
With trust drivers identified in Phase 1, the next step was to translate those insights into actionable product features and interaction flows. This phase focused on understanding what users expect from remote consultations and co-creating solutions that could reduce hesitation and encourage adoption.
Interview & Co-creation Flow - Generative, Participatory



Expectation Mapping
Co-creation Sessions
Concept Validation
What information, interface cues, or interactions would make users feel confident booking a video consultation?
Using guided “what-if” scenarios, participants co-created feature ideas that addressed their anxieties.
(“If the app showed doctor credentials/testimonials upfront, would that help? What else would you want to see?”)
Follow-up discussions assessed whether these proposed features aligned with user expectations and actually reduced trust-related hesitation.
What This Phase Delivered
-
A prioritized set of design levers (e.g., visible doctor credentials, verified patient testimonials, warm onboarding messaging) directly linked to user trust needs
-
Insights-to-Design Mapping, connecting each persona’s key barrier to a specific product or content recommendation—ensuring all user types were considered in feature ideation
03. From User Voices to Trust Patterns
Analysing what Builds (or Breaks) Trust
What drives or breaks trust in remote care? To answer this, I analyzed hours of interviews, coded hundreds of user statements, and looked for repeating emotional triggers.
01
Decoding Conversations to Surface User Pain Points
Coding and Transcription
I started by coding every interview line by line, tagging trust-building and trust-eroding cues. Patterns like doubts about diagnostic accuracy or skepticism toward online expertise began surfacing repeatedly across users
In person, doctors ask detailed questions, check me properly, and explain what’s happening. Their confidence makes me feel safe.
→ Code 1: Trust Driver – Detailed Examination
→ Code 2: Trust Driver – Clear Communication
I tried consulting a doctor online once but I didn’t feel very confident. It felt rushed, like the doctor was just trying to finish quickly. He only asked me some basic questions and prescribed. The examination wasn't thorough.
→ Code 1: Adoption Barrier – Impersonal Experience
→ Code 2: Adoption Barrier – Perceived Carelessness
To decide which doctor to meet online, I’d need to see their qualifications clearly and maybe some patient reviews. Without that, I keep wondering, “Who is this doctor really?”
→ Code 1: Trust Cue – Credentials Online
→ Code 2: Trust Driver – Peer Validation (Digital)
But scattered pain points alone weren’t enough.
The next step was to organize these fragments into meaningful themes.
02
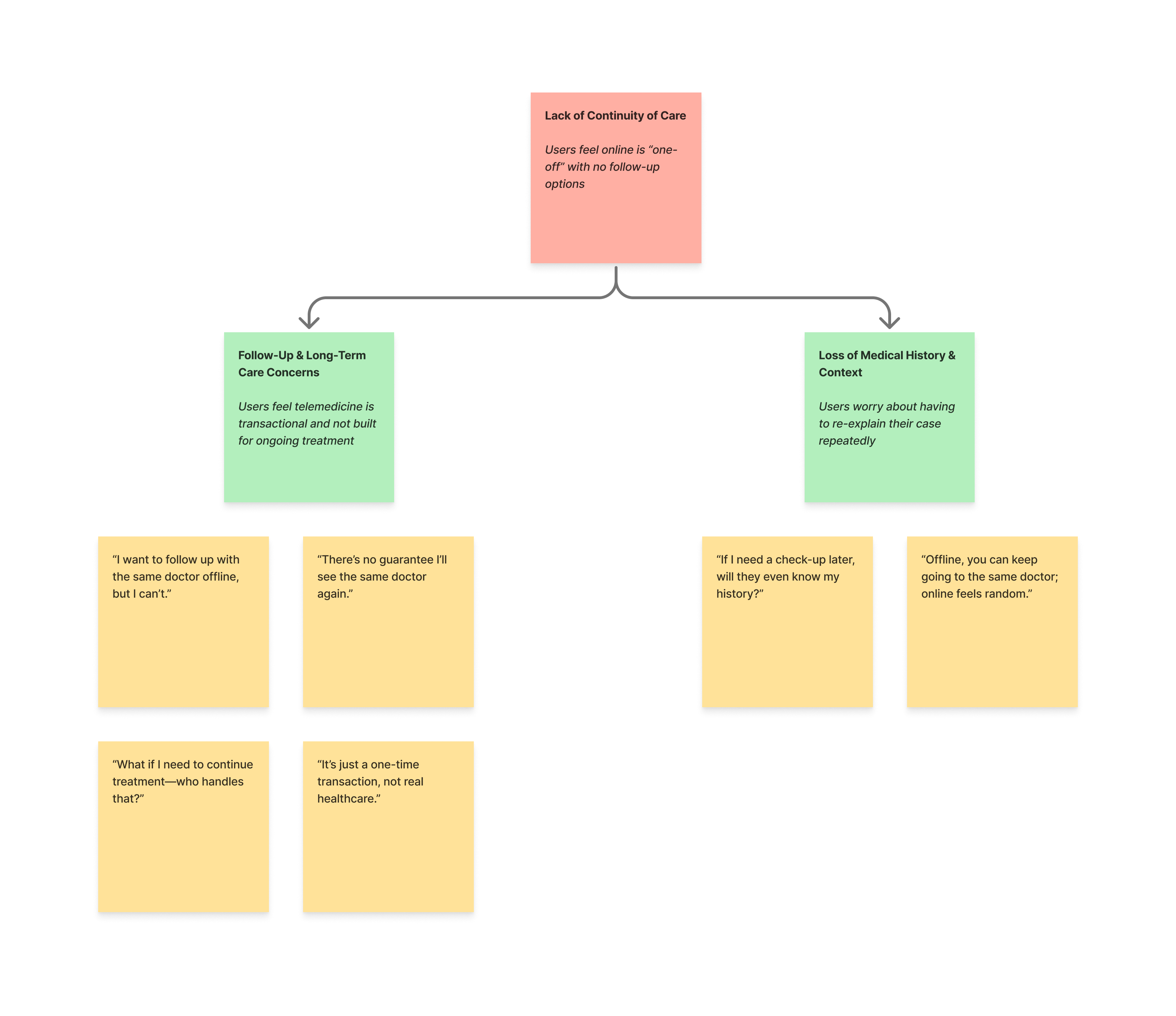
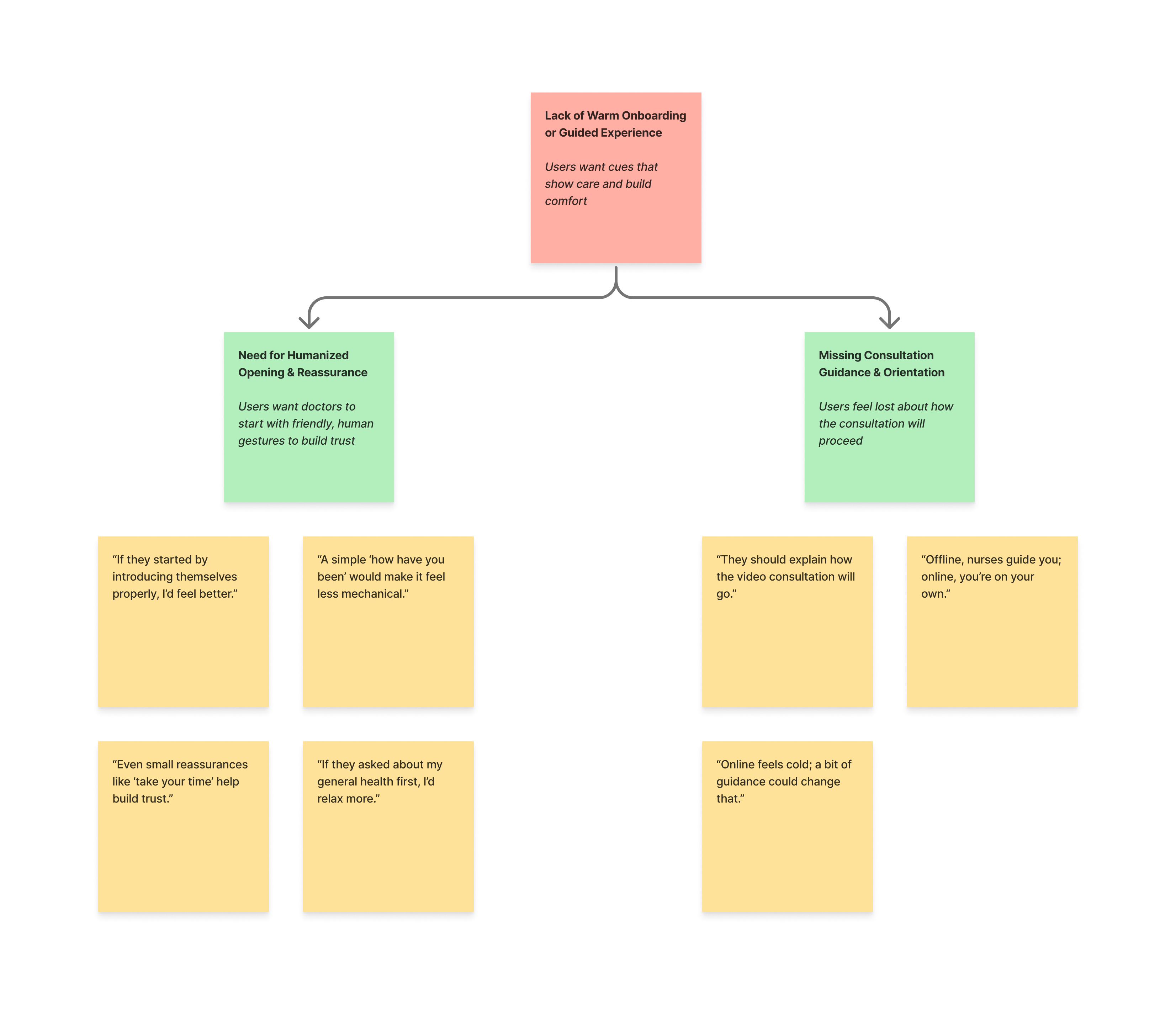
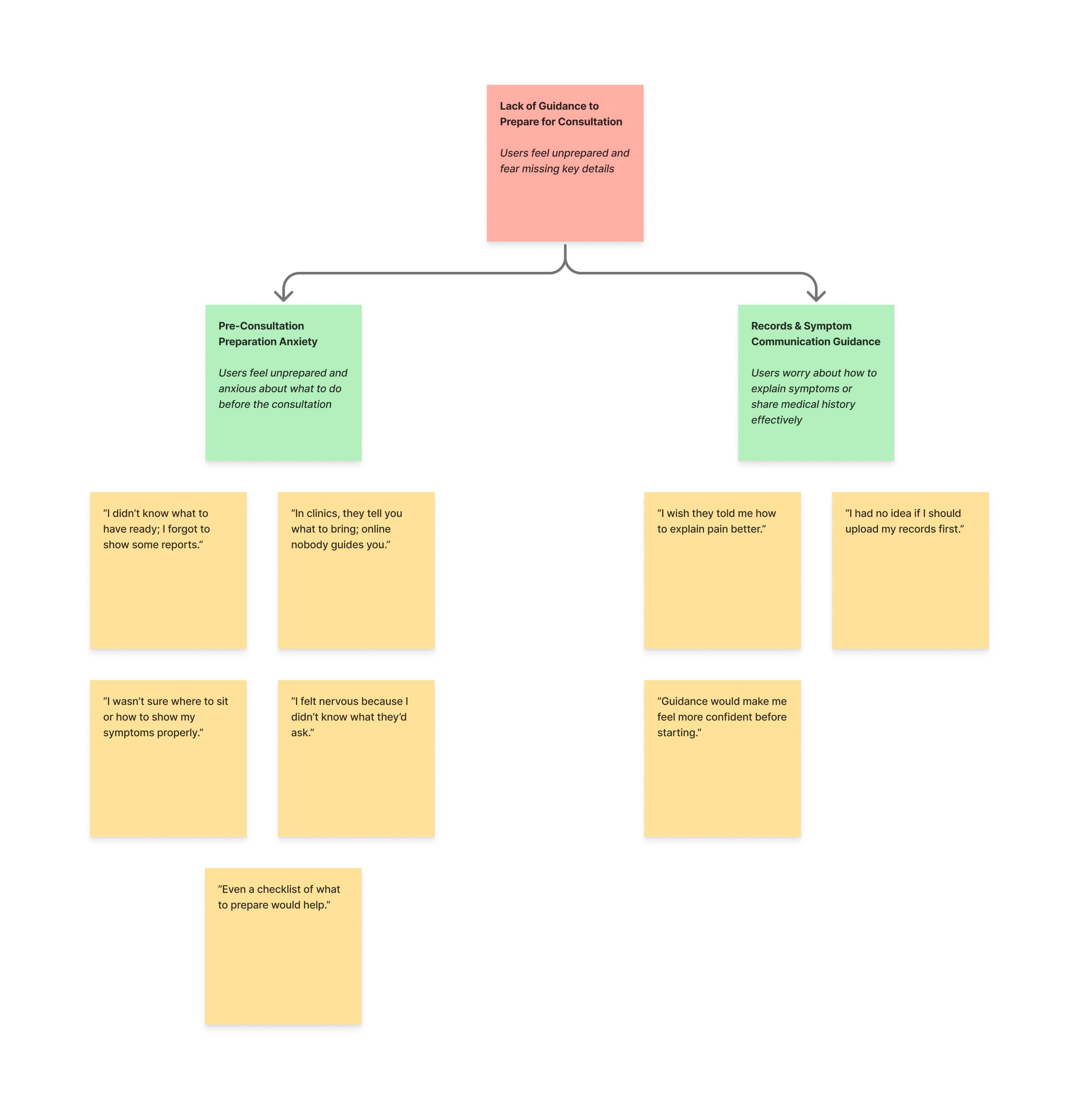
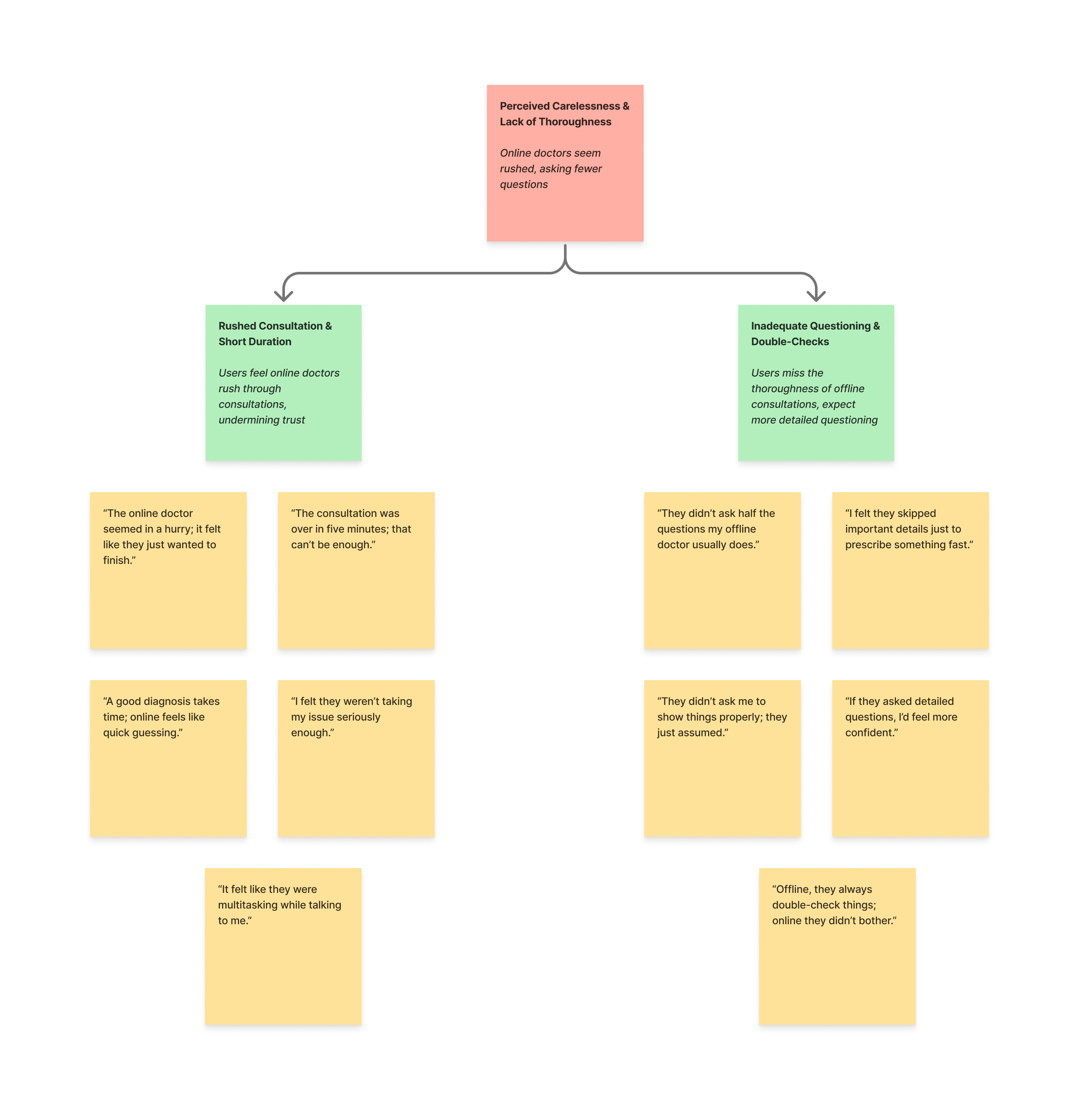
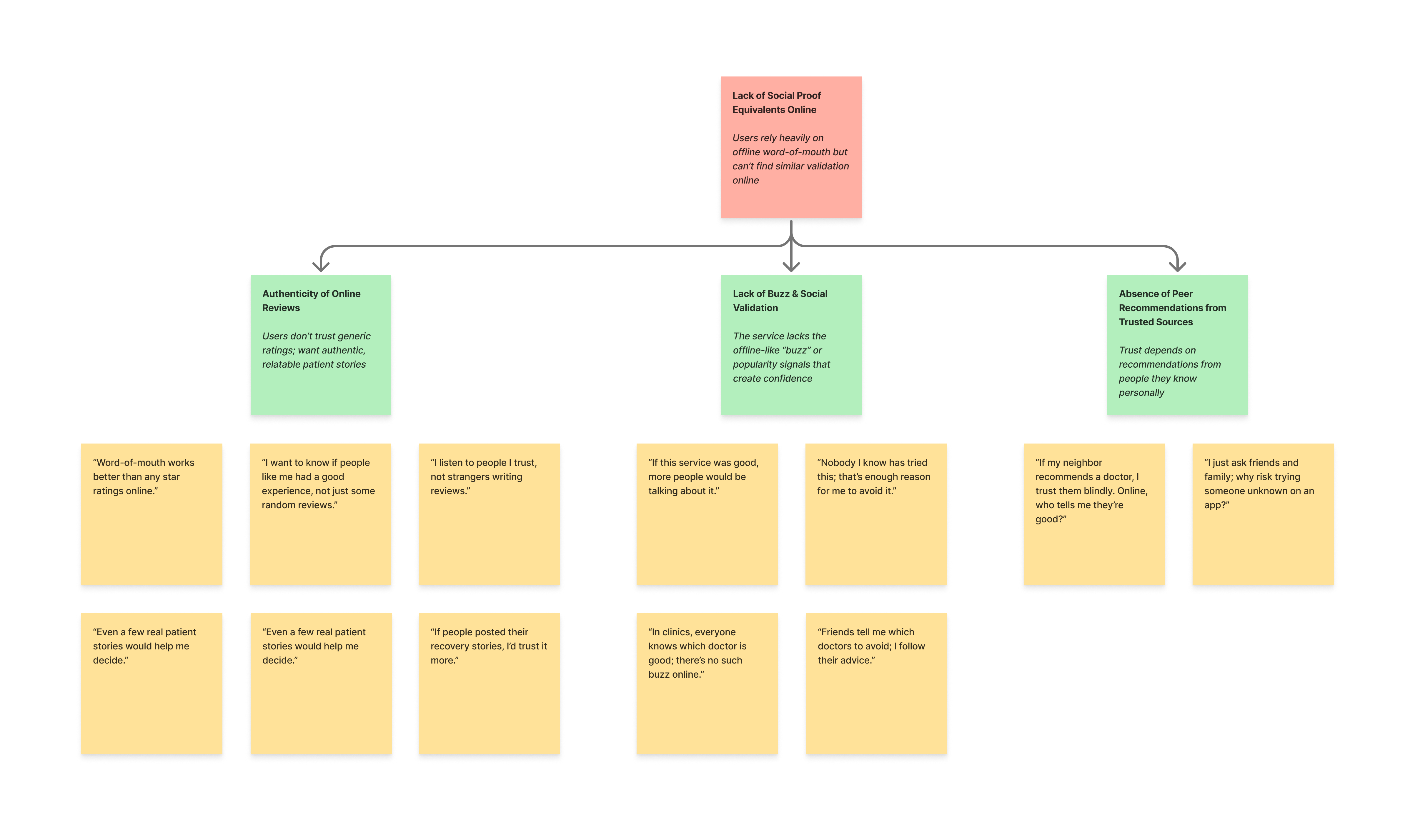
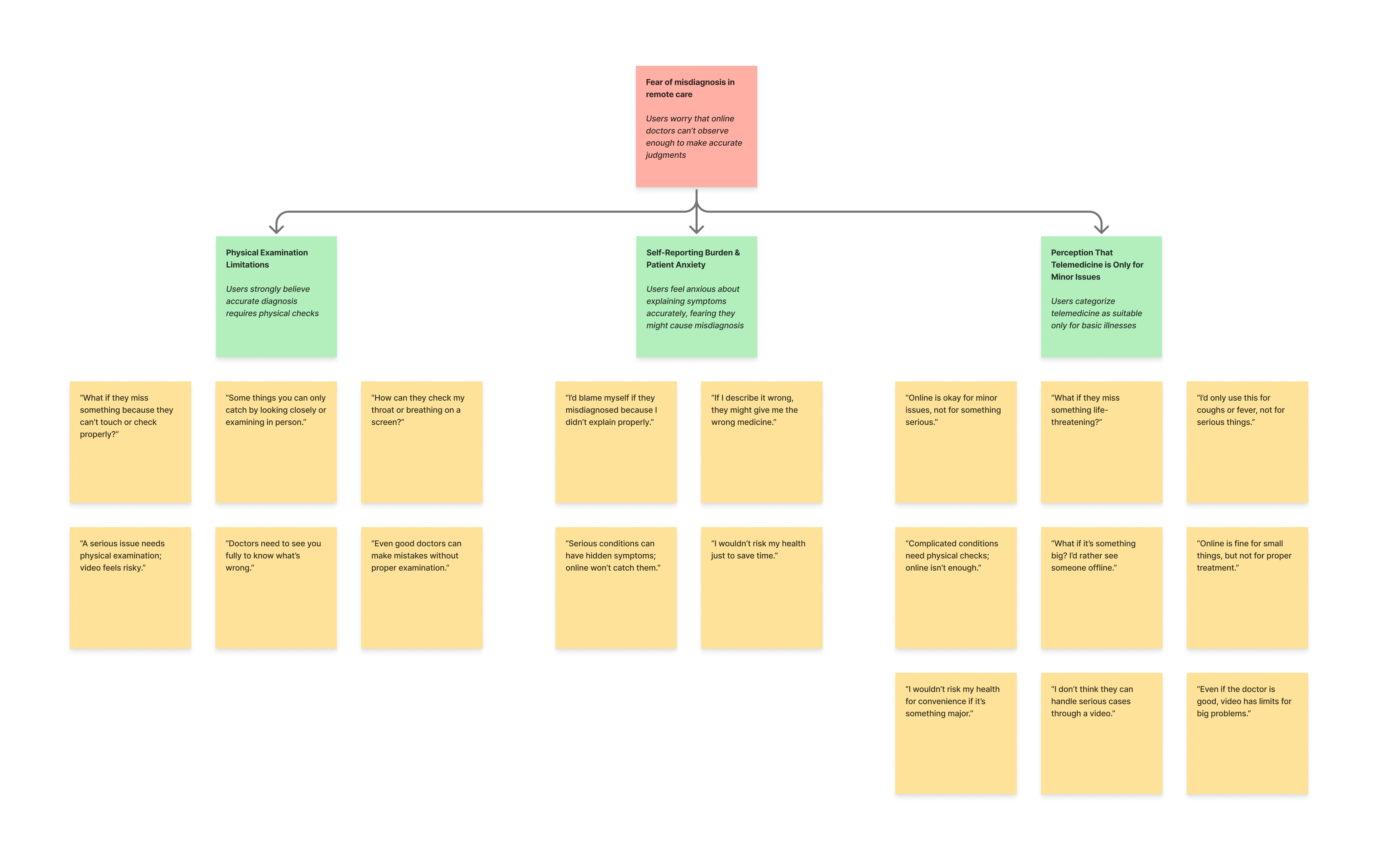
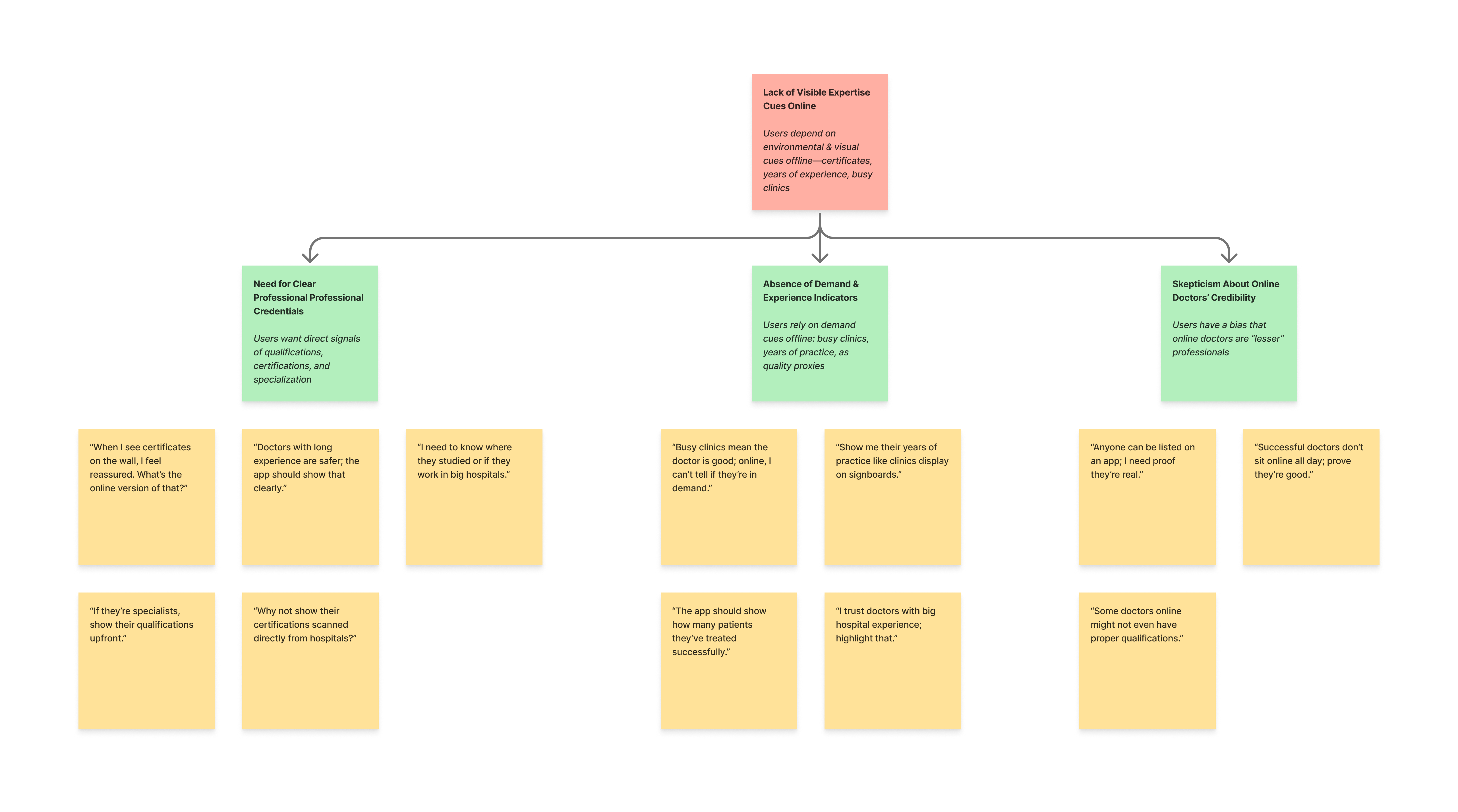
From Scattered User Pain Points to 9 Clear Trust Barriers
Affinity Mapping
Using affinity mapping, I clustered similar pain points into themes, gradually revealing 9 distinct barriers that either built or eroded trust in remote care. These barriers ranged from the absence of visible expertise to the fear of misdiagnosis.
However, barriers weren’t experienced the same way by everyone. To design effectively, I needed to understand who these users were and how their attitudes shaped their trust decisions.
03
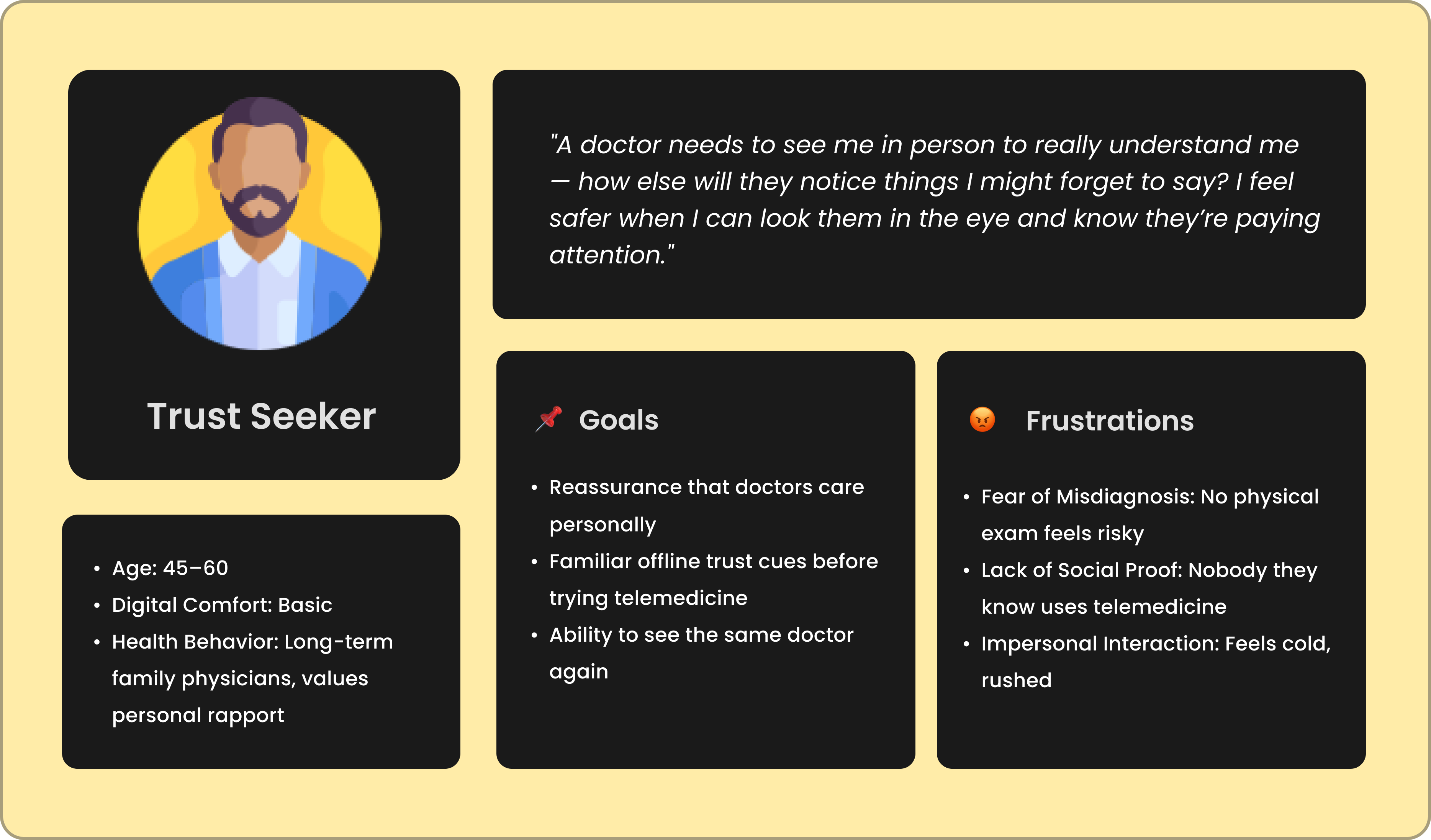
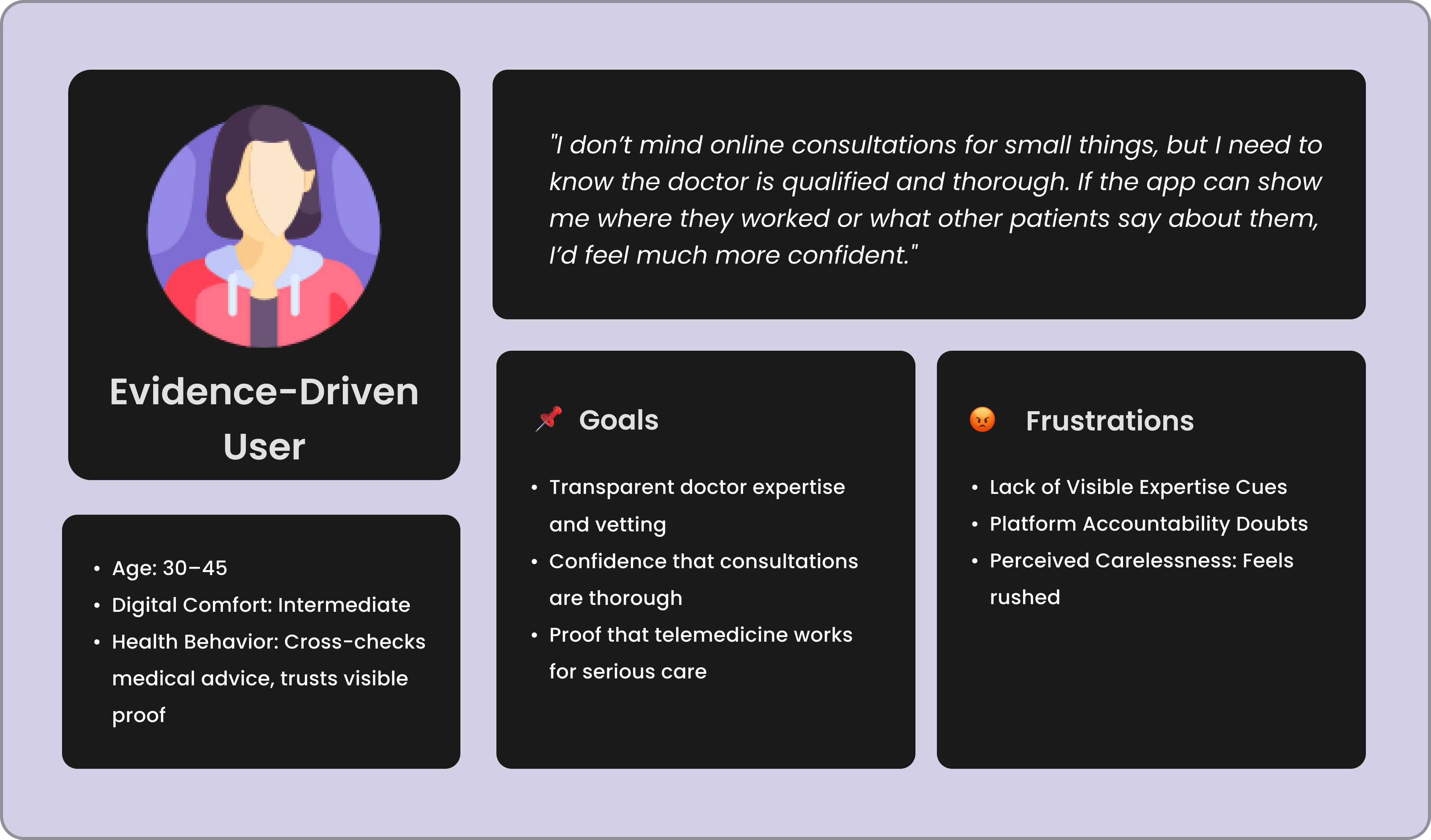
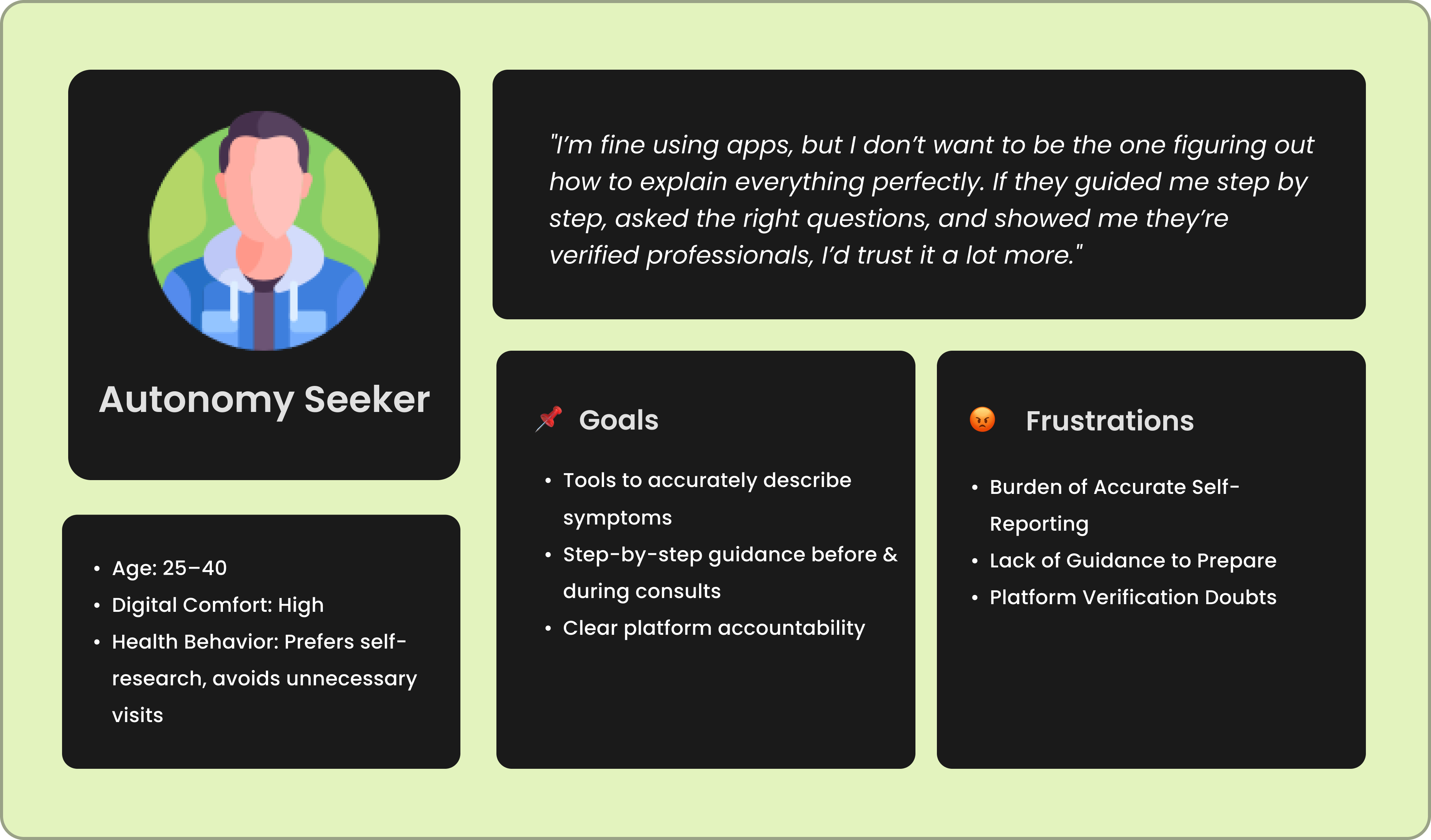
Three Distinct Trust Achetypes Emerged
User Personas
By analyzing behavioral and attitudinal patterns, I identified three user personas - the Trust-Seeker, the Evidence-Driven User, and the Autonomy-Seeker. Each represented a unique mindset toward telemedicine, from cautious first-timers to pragmatic, control-driven users.
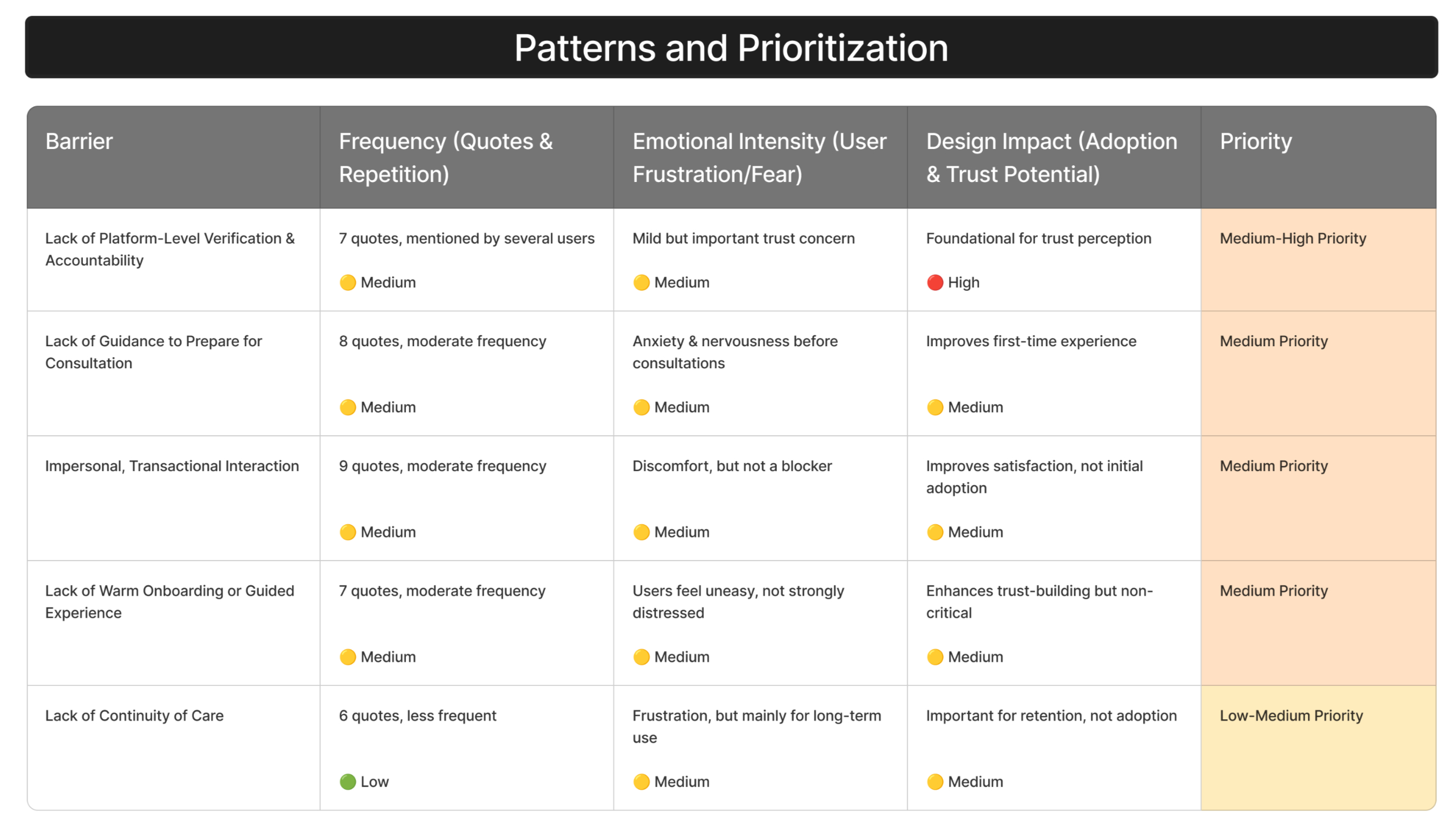
With clear barriers and user archetypes, the next step was to prioritize what truly mattered for adoption, not every frustration equally impacted trust.
04
Prioritizing What Matters The Most for Adoption and Trust
Pattern Prioritization
Using frequency, emotional intensity, and potential design impact as criteria, I prioritized the 9 barriers. Four emerged as high-priority trust blockers, becoming the core focus for design interventions.
With the key barriers defined, the next challenge was to translate these insights into actionable design opportunities, starting with understanding what users expected across their journey.
04. Turning Insights Into Design Ideas
Identifying what drives or erodes trust was only half the work; the real challenge was translating these insights into solutions users would actually trust. In this stage, I mapped user expectations across their teleconsultation journey, co-created and validated feature ideas with them, and finally distilled everything into clear design recommendations, each rooted in a real user quote and a validated trust barrier.
01
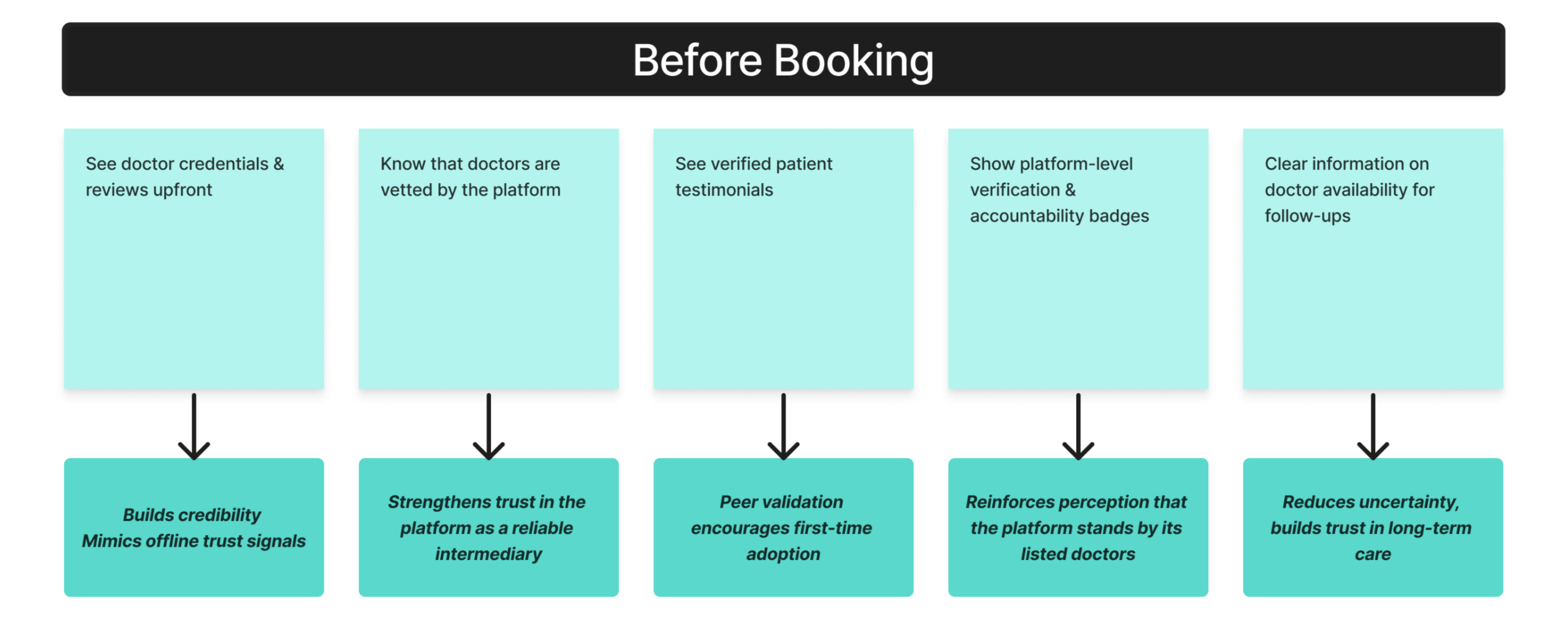
What Users Expected: Mapping Trust Levers Across the Journey
Expectation Mapping
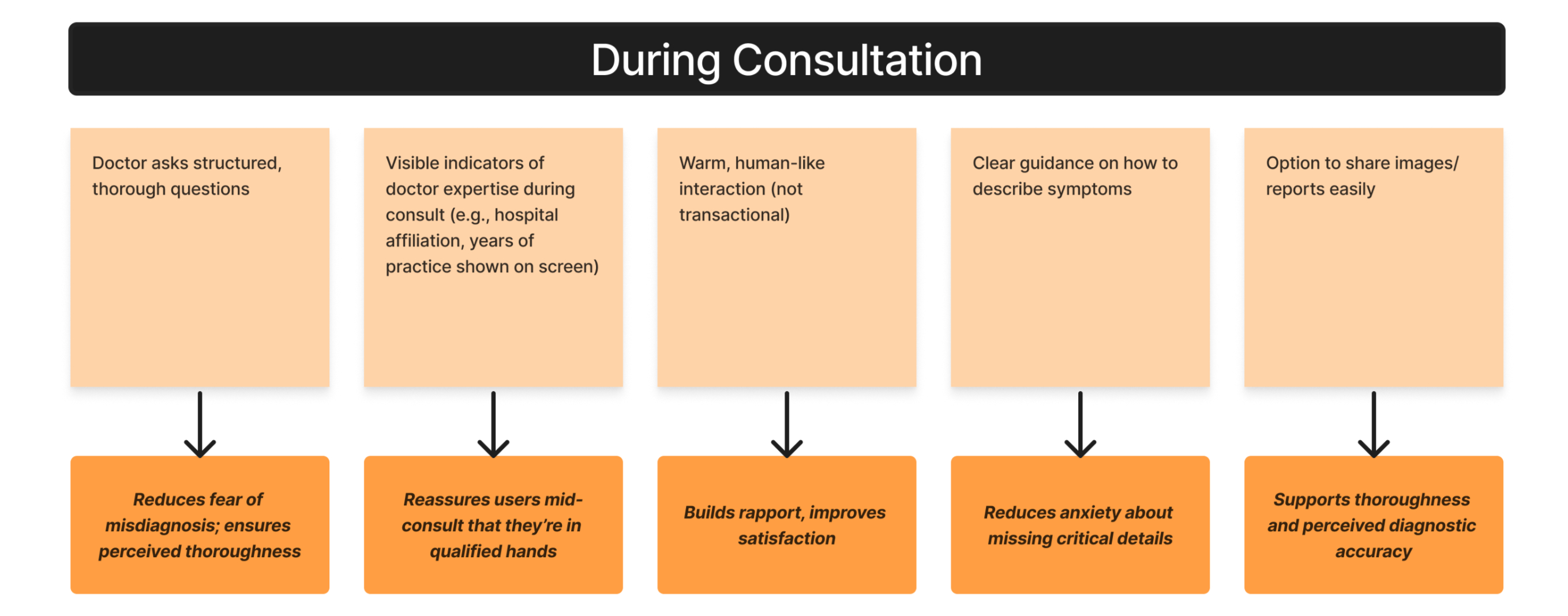
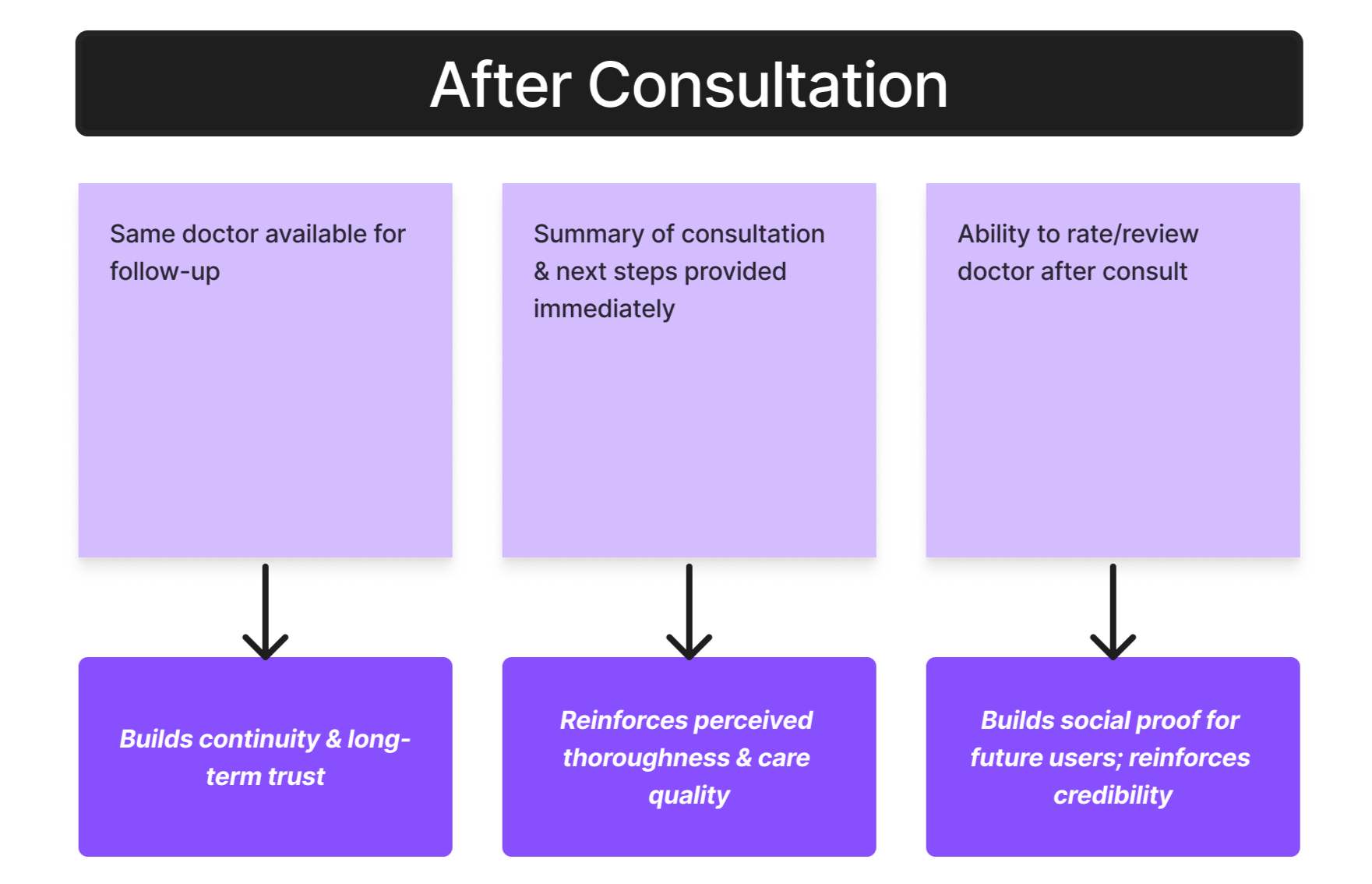
If we wanted to design for trust, I first needed to know: what signals make users feel confident at different stages of the teleconsultation journey? I mapped user expectations across the journey, before booking, during consultations, and after, revealing trust levers like visible expertise, structured questioning, and continuity of care.
But knowing what users expected wasn’t enough. The next step was to collaborate with them to turn these trust levers into concrete feature ideas.
02
Co-Creating & Validating Solutions With Users
Co-creation Sessions
I facilitated co-creation sessions using “what-if” scenarios and quick sketching prompts, asking users to imagine features that would reduce their hesitation. Over multiple sessions, we co-created 20+ ideas.
To separate “nice-to-haves” from “must-haves,” we validated these ideas in follow-up interviews, using dot-voting to rate their trust-building potential.
With validated ideas in hand, it was time to translate them into clear design recommendations, showing stakeholders how every quote and barrier directly informed a feature.
05. Designing the Solutions
Every feature recommendation was rooted in research — starting from a user quote, tied to a trust barrier, and validated for its impact. Below, you’ll see how these insights translated into specific design proposals aimed at building confidence across the teleconsultation journey
Before Booking Consultation

“If I can’t even see where the doctor works or what experience they have, how do I know they’re legit?”
Barrier
Lack of Visible Expertise Cues
Solution
Doctor profile cards with verified credentials, hospital affiliation, and years of experience prominently displayed.
Why it Works
Mimics the offline cues users trust
Users It Impacts

“People like me have used this doctor? That would convince me to try it.”
Barrier
Lack of Social Proof Online
Solution
Verified patient testimonials & treatment outcomes, with the option to see people with similar profiles who booked this doctor.
Why it Works
Uses peer validation, especially for first-time users.
Users It Impacts

“I just want to know this app takes responsibility for the doctors listed!”
Barrier
Lack of Platform-Level Verification & Accountability
Solution
Platform verification badge with a short explanation of the vetting process.
Why it Works
Builds trust in the platform as a reliable intermediary, not just a listing service.
Users It Impacts
During Doctor Consultation

“What if they miss something? A good doctor always asks lots of questions in person.”
Barrier
Fear of Misdiagnosis in Remote Care
Solution
Structured question flow; body diagram to indicate areas affected
Why it Works
Makes the consultation feel as thorough as offline visits, directly reducing fear of misdiagnosis.
Users It Impacts

“If they just act formal and cold, I won’t trust them… feels like I’m just another case.”
Barrier
Impersonal, Transactional Interaction
Solution
Doctors ask personal context questions (“How are you feeling today?”) + optional health background note from users.
Why it Works
Humanizes the interaction and builds rapport quickly, which users associated with trust.
Users It Impacts

If I saw which hospital they’re linked to while we talk, I’d feel safer trusting them.
Barrier
Lack of Visible Expertise Cues During Consult
Solution
Hospital/clinic logo displayed during consult + doctor’s credentials visible in-call.
Why it Works
Subtle but powerful reminder of the doctor’s credibility during diagnosis.
Users It Impacts
After Doctor Consultation

“I always forget what the doctor said. A written plan would help.”
Barrier
Perceived Carelessness & Lack of Thoroughness
Solution
End-of-consult summary + recommended next steps checklist, auto-shared after every consult.
Why it Works
Signals thoroughness and care, helping users feel their case is managed professionally.
Users It Impacts

“I don’t want to explain everything all over again if I book again!”
Barrier
Lack of Continuity of Care
Solution
Book same doctor again” button + doctor notes carried forward to next consult.
Why it Works
Mimics the familiarity of offline care, which was a strong trust trigger for repeat users.
Users It Impacts

“It’d feel safer if I could ask one or two follow-up questions after the consult.”
Barrier
Perceived Carelessness & Lack of Thoroughness
Solution
Option to message doctor for 24 hours post-consult + Doctor's recommendation checklist
Why it Works
Extends perceived care beyond the consult, increasing confidence in the diagnosis.
Users It Impacts
Each of these solutions directly maps to a validated trust barrier and was co-created with users. By designing for these trust levers, we aimed to replicate the credibility and reassurance of offline care in a digital environment—building confidence at every stage of the teleconsultation journey.
06. Impact at a Glance
70%
increase in video consultation adoption over 3 years after implementing trust-building features.
9
key trust barriers identified & prioritized, with 4 high-priority ones directly influencing adoption decisions.
20+
co-created feature ideas validated with users, ensuring solutions were research-backed and adoption-ready.
3
trust archetypes defined, enabling targeted design solutions for different user attitudes toward telemedicine.
07. What I Bring to Future UX Projects
This project honed my ability to connect deep user understanding with actionable design recommendations that drive product adoption.